

Critical care medicine specialists are responsible for diagnosing and treating a diverse range of diseases. Caring for critically ill patients requires a multidisciplinary team approach. However, reporting critical care services can be challenging due to the complex rules and regulations involved. As a medical billing and coding company, we stay current on these guidelines to ensure that clients’ services are reported correctly on claims.
Both Medicare and commercial payers closely examine how critical care services are billed. Accurate and detailed documentation is essential when reporting these services. Proper documentation not only ensures appropriate reimbursement but also helps convey the complexity and intensity of the care provided.


Take the first step toward efficient critical care medical billing and coding
Medicare’s guidelines now align with the CPT’s definition of critical care, which states that it involves the care of a critically ill or injured patient with acute impairment of one or more vital organ systems, resulting in a high probability of imminent or life-threatening deterioration. Additionally, critical care requires complex decision-making to address single or multiple vital organ system failures and to prevent further life-threatening deterioration (Physicians Practice, 2023).
Critical care services can be provided by physicians and non-physician practitioners (NPPs), including nurse practitioners (NPs), physician assistants (PAs), certified nurse specialists (CNSs), and certified nurse midwives (CNMs). In 2022, CMS specified that critical care services may be reported by a physician or non-physician practitioner (NPP) who is a QHP. According to CMS, a QHP is “an individual who is qualified by education, training, licensure/regulation (when applicable), facility privileging (when applicable),” working within their scope of practice. Medicare acknowledges that PAs can directly bill under their own National Provider Identifier (NPI) and receive direct payment for their professional services. It is important to ensure that each provider is properly credentialed to deliver services within the hospital where they are treating patients.
Since critical care services are time-based, it’s crucial to document the total time spent providing direct critical care to the patient. In 2024, a significant number of CPT updates are related to time-based codes.
There are two CPT codes to report critical care services:
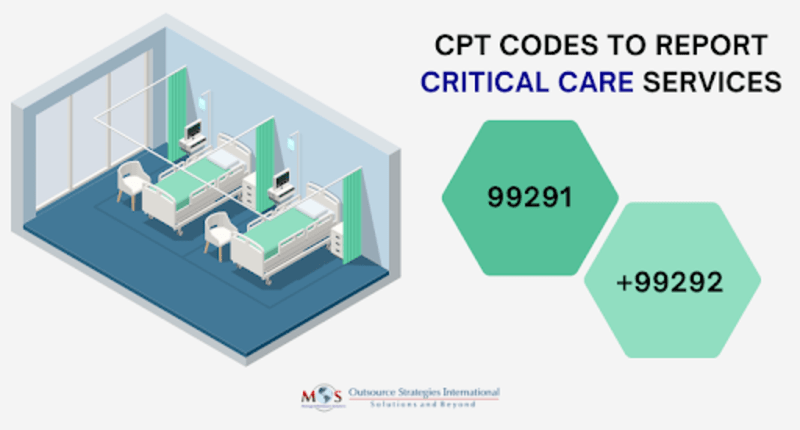
99291 Critical care, evaluation and management of critically ill or critically injured patient; first 30-74 minutes.
+99292 Critical care, evaluation and management of critically ill or critically injured patient; each additional 30 minutes (list separately in addition to code for primary services).
These codes report the total duration of critical care time (continuous or aggregated) provided by the physician or other QHP for a given date of service. Time spent performing separately reportable procedures or services should not be included in the time reported as critical care time.
Though the CPT Panel changed the code descriptors for office and hospital E/M codes in 2024 to include a minimum time for reporting the code instead of a time range, the critical care code (99291, 99292) descriptors continue to include time ranges.The following chart from the American College of Surgeons January 2024 Bulletin highlights the CPT and Medicare reporting guidelines for these services:
CPT vs. Medicare Reporting for Critical Care Services
| Total Duration of Critical Care Services | CPT Reporting Instructions | Medicare Reporting Instructions |
| Less than 30 minutes | 99221, 99231-99233 as appropriate | 99221-99231, 99231-99223 as appropriate |
| 30-74 minutes | 99291 x 1 | 99291 x 1 |
| 75-104 minutes | 99291 x 1 and 99292 x 1 | 99291 x 1 |
| 105-134 minutes | 99291 x 1 and 99292 x 2 | 99219 x 1 and 99292 x 1 |
| 135-164 minutes | 99291 x 1 and 99292 x 3 | 99291 x 1 and 99292 x 2 |
| 165 minutes or longer | 99291 and 99292 |
Source: ACS Bulletin, January 10, 2024
CPT 2022 bundled several services into critical care services, making them not separately payable when furnished concurrently with critical care. Do not report these services in addition to the critical care service codes.
Bundled services include:
All services need to be sufficiently documented to determine the role each practitioner plays in the treatment of the patient’s care. It is important to report the time spent performing separately reportable procedures or services separately, and not include it in the time reported as critical care time.
Modifier 24 (Unrelated evaluation and management service) or modifier FT (Unrelated evaluation and management visit) should be used when billing critical care services to indicate that the critical care was unrelated to the procedure. Modifier FT is mandatory on claims starting from March 1, 2022.
If critical care is performed in the postoperative period by a provider other than the surgeon, a modifier is not required. However, if the care is fully transferred from the surgeon to an intensivist and the critical care is unrelated, modifiers 54 (Surgical care only) and 55 (Postoperative management only) must be reported, as stated by CMS in the final rule.
When reporting critical care services, practitioners must document:
Providers need to be familiar with Medicare and private payer rules and policies on billing critical care services.It is also critical to avoid over utilization and unbundling services inappropriately, billing for critical care when the patient does not meet the critical care definition, and other high-risk coding behavior. Partnering with a competent provider of critical care medical coding services is a feasible option to ensure accurate and thorough documentation of these services for optimal reimbursement.
Ensure accurate reimbursement and compliance with our expert medical billing services.